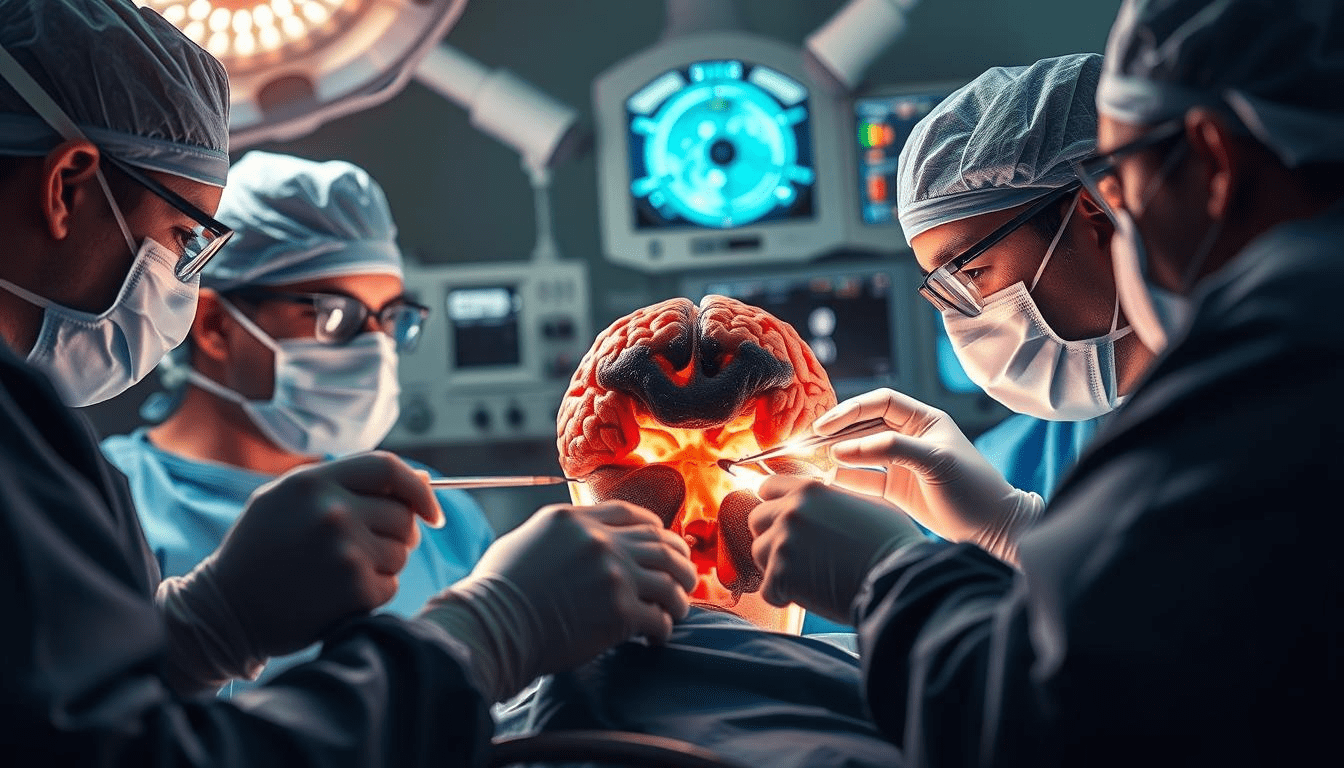
For patients diagnosed with a brain tumor, surgery is often the critical first step toward treatment. The primary goals are clear: achieve the maximal possible removal of the tumor while meticulously preserving healthy brain tissue and neurological function. Today, Brain Tumor Surgery is not a single procedure but a suite of advanced, synergistic technologies that have transformed it into a discipline of remarkable precision, safety, and effectiveness.
The Guiding Principle: Maximal Safe Resection
The cornerstone of modern Brain Tumor Surgery is the concept of maximal safe resection. Neurosurgeons aim to remove as much of the tumor as is safely possible, as this is consistently linked to better outcomes and longer survival. The “safe” component is paramount. To navigate the brain’s delicate landscape, surgeons now operate with an array of sophisticated tools that act as their eyes, ears, and GPS.
Key Modern Techniques Enhancing Safety and Precision
-
Advanced Preoperative Imaging and Planning: Surgery begins long before the first incision. High-resolution MRI scans, including functional MRI (fMRI) and diffusion tensor imaging (DTI), are used to create a detailed 3D map of the brain. This map identifies the tumor’s exact boundaries and, crucially, pinpoints critical functional areas (like those for speech or movement) and major nerve pathways that must be protected.
-
Intraoperative Neuronavigation: Think of this as a real-time GPS for the brain. Using the preoperative 3D map, this computer-guided system shows the surgeon’s exact instruments in relation to the tumor and vital brain structures on a monitor, allowing for unparalleled accuracy in planning the surgical approach and tracking progress.
-
Intraoperative Neurophysiological Monitoring (IONM): This is the surgeon’s “live feedback” system. During surgery, specialized neurologists stimulate nerves and monitor brain activity in real-time. If an area responsible for movement or speech is approached, the monitoring team can alert the surgeon immediately, helping to prevent unintended neurological injury.
-
Awake Craniotomy: For tumors located in or near eloquent brain regions (like those controlling speech or motor function), an awake procedure may be recommended. The patient is awakened after the skull is opened. The surgeon can then safely map the brain by interacting with the patient asking them to speak, move a hand, or identify pictures while removing the tumor. This direct feedback is the gold standard for preserving essential functions.
-
Fluorescence-Guided Surgery: In certain tumor types, the patient is given a special fluorescent dye (like 5-ALA) before surgery. This dye is absorbed by tumor cells, causing them to glow a vivid pink under a specialized microscope light. This visual contrast helps the surgeon distinguish tumor tissue from healthy brain, aiding in more complete removal.
A Team Effort for Recovery
Modern Brain Tumor Surgery is a team endeavor. The neurosurgeon works alongside neuro-anesthesiologists, neuro-monitoring specialists, and oncology nurses. This collaborative approach extends into recovery, where early rehabilitation is often integrated to help patients regain strength and function.
The field of Brain Tumor Surgery has moved far beyond simply opening the skull. It is now a highly sophisticated integration of imaging, real-time mapping, and monitoring technologies. These advances collectively empower surgeons to operate with greater confidence, offering patients safer procedures, more effective tumor removal, and the best possible foundation for recovery and subsequent treatments.